Obsessive-Compulsive Disorder, commonly known as OCD, is a complex mental health condition. It’s characterized by recurring, unwanted thoughts and repetitive behaviors.
As with all mental health conditions, understanding the symptoms of OCD is crucial for early detection and intervention. This knowledge can also help in supporting those living with the condition.
I want to talk today about the common and also lesser-known symptoms of OCD, how they manifest and their impact on daily life.
I’ll also discuss the latest research findings on OCD symptoms to give you a good understanding of the condition.
Whether you’re a mental health professional, someone suspecting they might have OCD, or a loved one seeking to understand, this article is for you.
The Nature of Obsessive-Compulsive Disorder
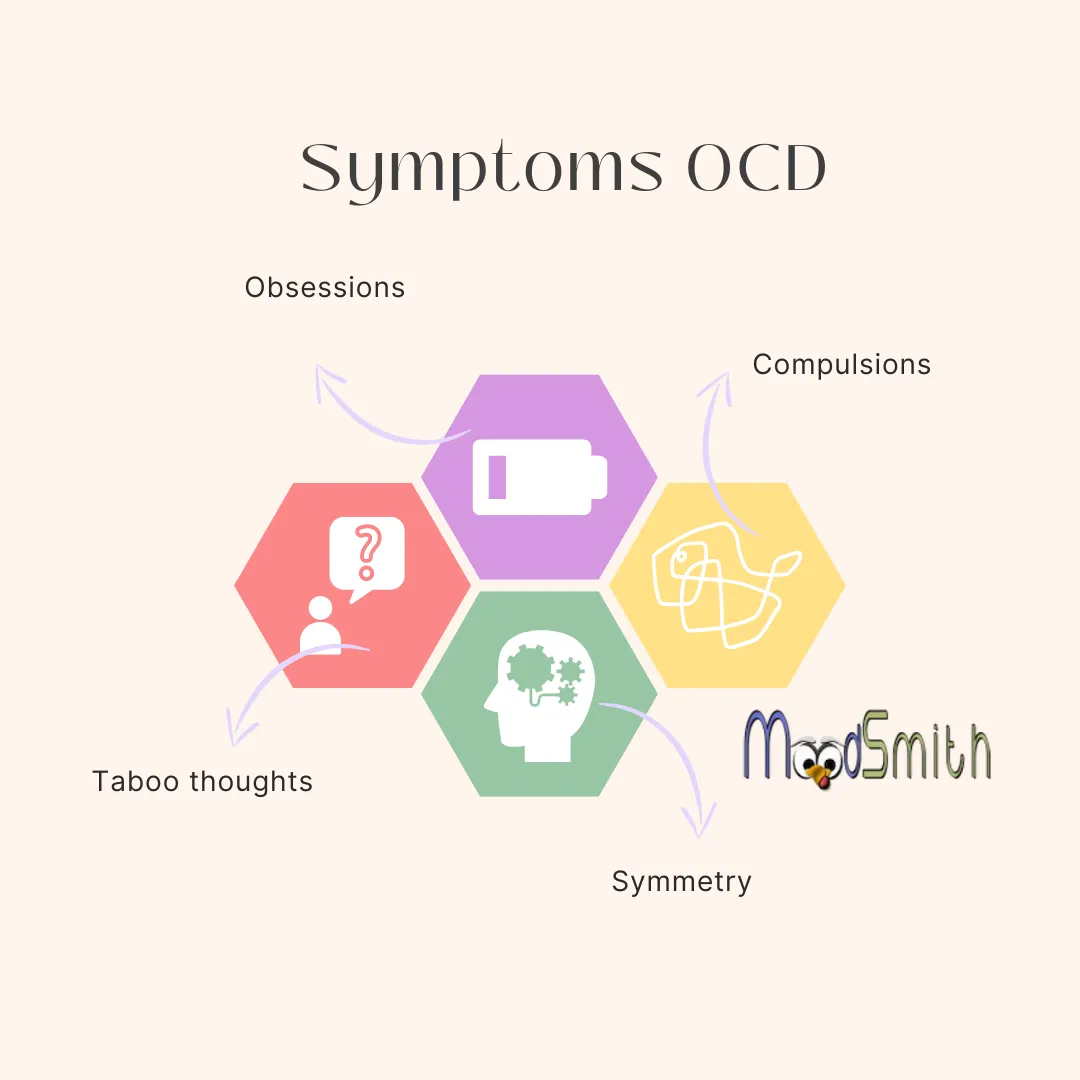
Obsessive-Compulsive Disorder (OCD) is a chronic anxiety disorder marked by obsessions and compulsions that interfere with daily life.
Obsessions are all those intrusive, unwanted thoughts that cause distress and the compulsions are repetitive behaviours or mental acts you do to make yourself feel better from the distress caused by the obsessions. For example you might obsess you could hurt someone, so you feel compelled to hide or dispose of things that can cause harm.
Defining OCD and Its Core Characteristics
OCD is more than just being overly neat or liking things in a certain order. It’s a serious mental health condition that can significantly impact a person’s quality of life.
Obsessions in OCD are persistent and unwanted thoughts, images, or impulses. They’re often disturbing and cause significant anxiety or discomfort.
Compulsions, on the other hand, are repetitive behaviours or mental acts. Individuals with OCD feel driven to perform these in response to an obsession or according to rigid rules.
The core characteristics of OCD include:
- Persistent and unwanted thoughts (obsessions)
- Repetitive behaviours or mental acts (compulsions)
- Significant distress or impairment in daily functioning
- Behaviours or mental acts aimed at preventing or reducing distress
Prevalence and Onset of OCD Symptoms
OCD affects about 2-3% of the world’s population. It’s a condition that doesn’t discriminate, affecting people of all ages, races, and socioeconomic backgrounds.
The average age of onset for OCD symptoms is around 19 years. However, it’s not uncommon for symptoms to appear in childhood or later in adulthood.
Recognizing the Symptoms of OCD
Recognizing the symptoms of OCD is the first step towards seeking help. Symptoms can vary widely among individuals, but they generally involve obsessions and compulsions.
Obsessions often revolve around certain themes, such as fear of contamination or making mistakes. Compulsions, on the other hand, are behaviours that individuals feel compelled to perform to alleviate the distress caused by obsessions.
Common Obsessions in OCD
Obsessions in OCD are intrusive and often distressing. They can take many forms, but some themes are more common.
Fears of contamination or germs are common obsessions in OCD. Individuals with these obsessions may fear becoming ill or spreading illness to others.
Another common obsession is the fear of harm or danger. This can involve fears of causing harm to oneself or others, often due to perceived negligence or forgetfulness.
Obsessions can also revolve around the need for symmetry or exactness. Individuals with these obsessions may feel distressed when objects are not arranged “just right” or if things are asymmetrical.
Common obsessions in OCD include:
- Fear of contamination or germs
- Fear of harm or danger
- Need for symmetry or exactness
- Fear of making mistakes or forgetting important information
Common Compulsions in OCD
Compulsions in OCD are repetitive behaviours or mental acts that individuals feel driven to perform. Like obsessions, compulsions often revolve around certain themes.
Washing and cleaning compulsions are common in individuals with fears of contamination. These can involve excessive hand washing, showering, or cleaning objects to prevent illness.
Checking compulsions are also common. These can involve repeatedly checking things, such as locks or appliances, to prevent harm or disaster.
Arranging or ordering compulsions are often seen in individuals with a need for symmetry or exactness. These can involve arranging objects in a certain way or performing tasks in a specific order.
Common compulsions in OCD include:
- Washing and cleaning
- Checking
- Arranging or ordering
- Repeating actions or rituals
Lesser Known Symptoms of OCD
While the above symptoms are common, there are also lesser-known symptoms of OCD. These can be just as distressing and disruptive, but they’re often overlooked or misunderstood.
Hoarding, for example, can be a symptom of OCD. Individuals with hoarding obsessions may fear that something bad will happen if they throw things away.
Symmetry obsessions and related compulsions are also lesser-known symptoms. Individuals with these symptoms may feel a need to perform actions symmetrically or to arrange objects in a symmetrical pattern.
Taboo thoughts, such as aggressive, sexual, or religious thoughts, are another lesser-known symptom. These thoughts are often disturbing to the individual and may be completely out of character.
Lesser-known symptoms of OCD include:
- Hoarding
- Symmetry obsessions and compulsions
- Taboo thoughts or mental images
Research Insights on OCD Symptoms
Research into OCD has provided valuable insights into the nature and variability of its symptoms. It has highlighted the complexity of the disorder and the need for personalized treatment approaches.
Variability and Evolution of Symptoms
One key finding is that the symptoms of OCD can vary widely among individuals. Some people may primarily experience obsessions, while others may struggle more with compulsions. The specific themes of these obsessions and compulsions can also differ greatly.
Furthermore, research indicates that the symptoms of OCD can change or evolve over time. An individual’s obsessions and compulsions may shift in response to stress, life changes, or treatment. This underscores the importance of ongoing monitoring and adjustment of treatment plans.
When to Seek Professional Help
If you or a loved one are experiencing symptoms of OCD, it’s crucial to seek professional help. OCD is a serious condition that can significantly impact daily life, but effective treatments are available.
In order to give you an idea what happens when you seek professional help, I have anonymised an old case study of mine that shall outline the process .
Example
Introduction Dr. Elaine Ryan is a psychologist specializing in cognitive behavioural therapy (CBT), with a strong focus on treating individuals with Obsessive-Compulsive Disorder (OCD). This anonymized case study provides an overview of the therapeutic approach using a composite character, “Alex”, who exhibits typical OCD symptoms.
Background Alex, a 30-year-old software developer, has struggled with OCD for several years. His symptoms primarily manifest as intrusive thoughts about contamination, which compel him to engage in excessive handwashing and cleaning rituals. These behaviours significantly disrupt his daily life, affecting his professional responsibilities and personal relationships.
Assessment Dr. Ryan begins her treatment with a thorough assessment, including a clinical interview and standardized questionnaires to gauge the severity of Alex’s OCD symptoms. She also evaluates Alex’s general mental health to identify any co-occurring disorders such as anxiety or depression, which are common in individuals with OCD.
Treatment Plan Based on the assessment, Dr. Ryan develops a personalized treatment plan for Alex, emphasizing Exposure and Response Prevention (ERP), that is highly effective for OCD. The plan includes:
- Education: Dr. Ryan educates Alex about OCD, explaining the nature of intrusive thoughts and the role of compulsive behaviors in reinforcing anxiety.
- Exposure Exercises: Alex is gradually exposed to situations that trigger his OCD symptoms but is encouraged to refrain from engaging in his usual compulsive behaviors. For example, he touches a doorknob and is asked to wait progressively longer before he is allowed to wash his hands.
- Response Prevention: Alongside exposure, Alex is taught to manage the anxiety that arises from not performing compulsive behaviors, using techniques such as deep breathing and mindfulness.
- Homework Assignments: Alex receives tasks to complete outside of sessions, ensuring that he applies the techniques in his daily environment.
Progress Monitoring Dr. Ryan regularly monitors Alex’s progress through follow-up sessions and adjusts the treatment plan based on his feedback and any changes in his symptom severity. Progress is quantitatively measured using the same questionnaires administered during the initial assessment.
Challenges and Adjustments Alex faces significant challenges during treatment, particularly the intense anxiety triggered by exposure exercises. Dr. Ryan supports him through these challenges by adjusting the pace of exposures and integrating additional support, such as group therapy sessions where Alex can share experiences and strategies with others facing similar issues.
Outcome After several months of consistent treatment, Alex reports a noticeable decrease in the frequency and intensity of his intrusive thoughts. His ability to resist compulsive behaviours improves, leading to a better quality of life both at work and home.
The Importance of Early Diagnosis and Intervention
Early diagnosis and intervention can greatly improve the prognosis for individuals with OCD. Timely treatment can help manage symptoms, prevent complications, and improve quality of life. It’s important not to delay seeking help if OCD symptoms are suspected.
Conclusion: Living with OCD
Living with OCD can be challenging, but with the right support and treatment, individuals can manage their symptoms and lead fulfilling lives. It’s important to remember that OCD is a medical condition, not a personal failing, and that help is available.
Further resources and reading on OCD